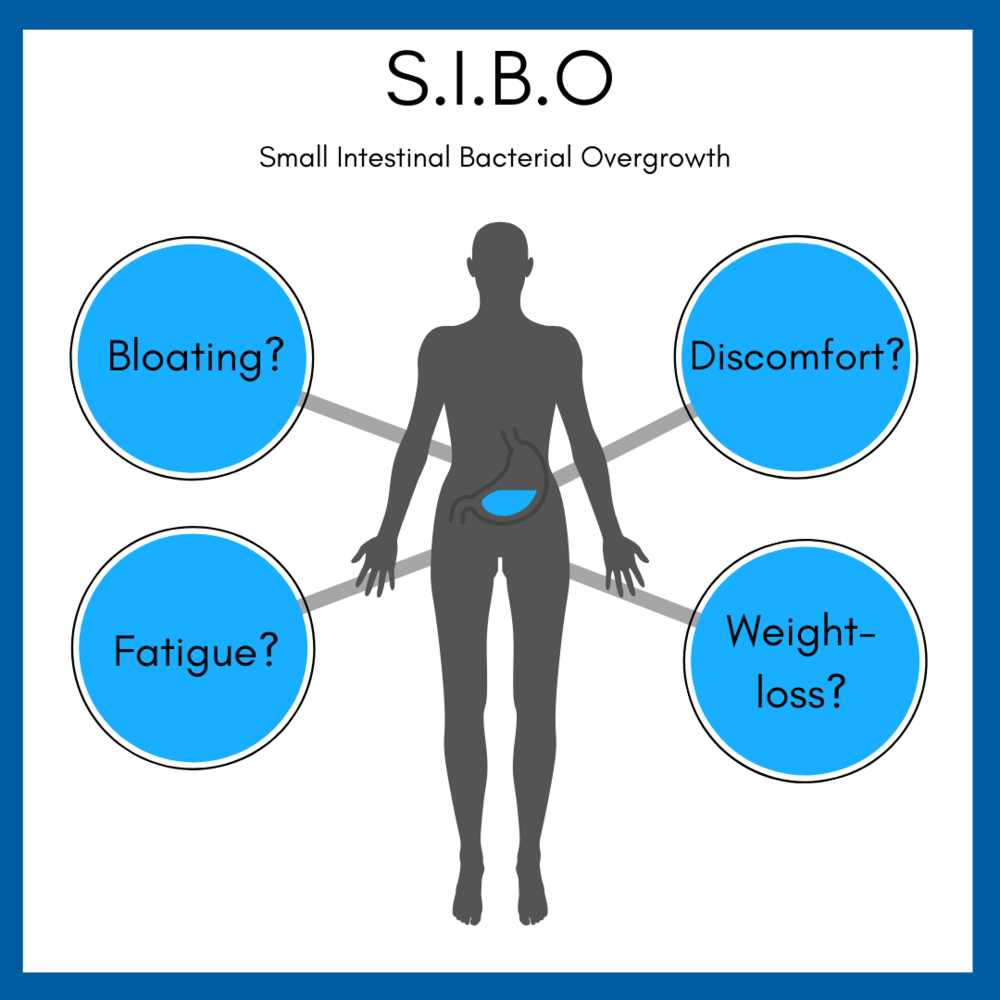
Small intestinal bacterial overgrowth (SIBO).
Small intestinal bacterial overgrowth (SIBO)
SIBO results when bacteria originating from the colon grow in excess in the small bowel. It can develop in patients with altered small bowel motility (eg, uncontrolled diabetes mellitus, chronic opiate use, scleroderma) or in those who have had surgery involving the ileocecal valve. Other predisposing conditions include small intestinal diverticula, chronic pancreatitis, and gastric hypochlorhydria (eg, chronic proton pump inhibitor use).
Patients typically have mild abdominal pain, bloating, flatulence, and watery diarrhea. Vitamin B12 deficiency is common due to bacterial consumption; however, folate levels may be elevated due to bacterial production of the nutrient.
The gold standard for diagnosis is a jejunal aspiration demonstrating a high bacterial concentration (eg, >103 colony—forming units/mL); however, this test is invasive and not easily performed. SIBO is more commonly diagnosed by a carbohydrate breath test using either glucose or lactulose. Patients with SIBO have an early peak in breath hydrogen/methane (due to carbohydrate metabolism by bacteria in the small intestine) compared to those without SIBO (in whom carbohydrate metabolism primarily occurs in the colon).
Treatment is with oral antibiotics (eg, rifaximin, neomycin) to reduce bacterial load.



