Blunt abdominal trauma
ABDOMINAL TRAUMA
Abdominal trauma caused by blunt force is a common presentation in the emergency room seen in adults and children. The chief cause of blunt abdominal trauma in the United States is motor vehicle accidents. This activity describes the clinical presentation, evaluation, and management of blunt abdominal trauma and the importance of the interprofessional team in educating patients on prevention of abdominal injuries.
Etiology
The chief cause of blunt abdominal trauma in the United States is motor vehicle accidents. Other rare causes include falls from heights, bicycle injuries, injuries sustained during sporting activities, and industrial accidents. In children, the most common causes are due to motor vehicle injuries and bicycle accidents
History and Physical
Because the presentation is often not straightforward, the diagnosis can be difficult and often time-consuming. Besides pain, the patient may present with bleeding per rectum, unstable vital signs, and the presence of peritonitis. The physical exam may reveal marks from a lap belt, ecchymosis, abdominal distention, absent bowel sounds and tenderness to palpation. If peritonitis is present, abdominal rigidity, guarding and rebound tenderness may be present. The mechanism of injury, motor vehicle speed, associated deaths at the scene, uses of alcohol or other substance of abuse must be taken into account so as not to miss an injury.
Evaluation
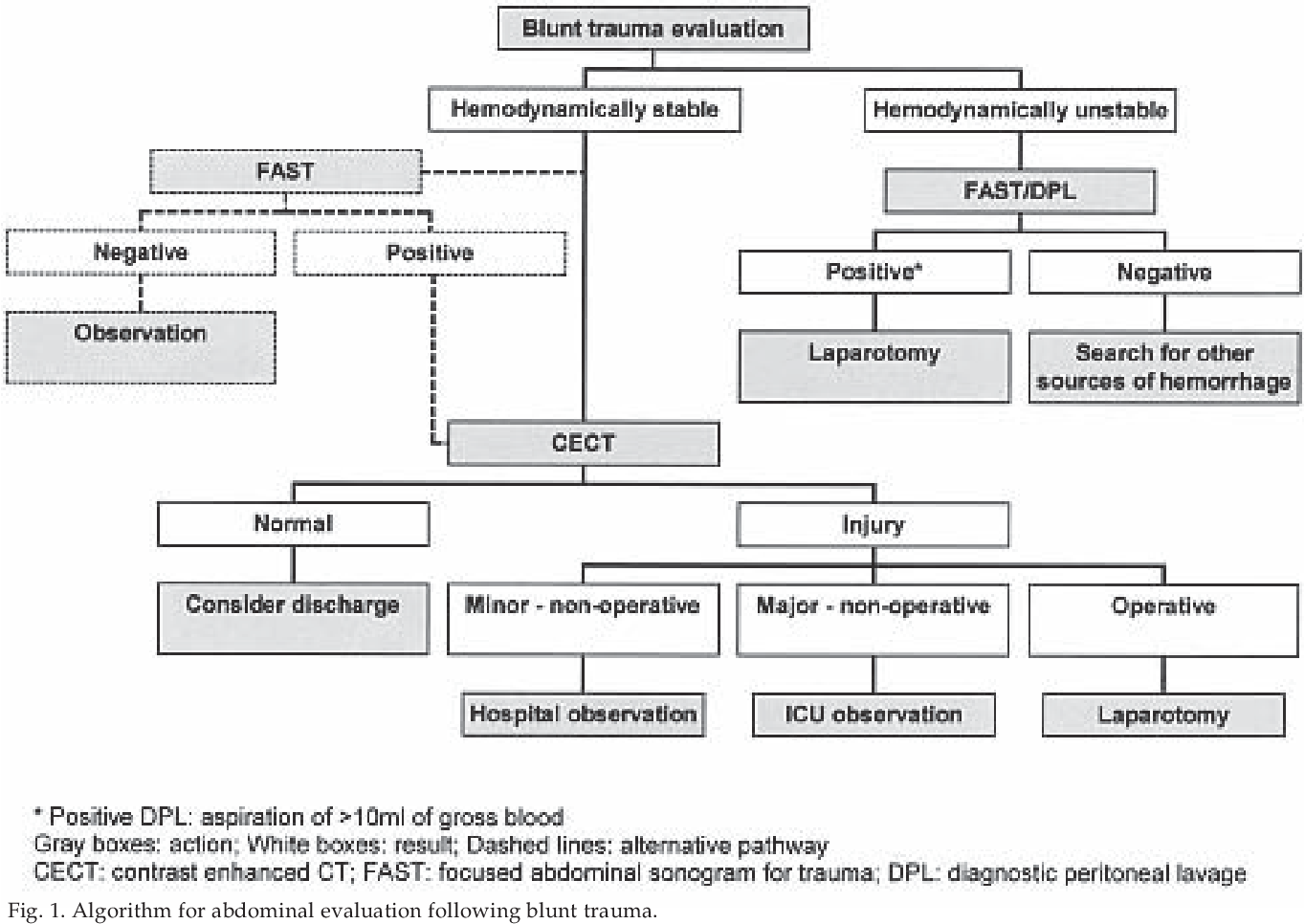
The evaluation of any trauma patient begins with evaluating the airway, accessing the breathing, and managing the circulation. The diagnosis of intra-abdominal injury following blunt trauma depends primarily on the hemodynamic status of the patient. If the patient is hemodynamically stable, CT scan is the ideal test to look for solid organ injury in the abdomen and pelvis. For unstable patients, one may perform an ultrasound (Extended Focused Assessment with Sonography for Trauma (EFAST)) or diagnostic peritoneal lavage, both of which are associated with a high rate of false negatives and false positives
The Extended Focused Assessment with Sonography for Trauma (EFAST) exam
1. RUQ (right upper quadrant)
2. Perisplenic space LUQ (left upper quadrant)
3. Pelvis (bladder)
4. Cardiac view
5. Normal Lung
Pearls and Other Issues
A-When a hollow viscus (eg, duodenum, ascending or descending colon) perforates within the retroperitoneum, gastrointestinal spillage may be initially sequestered away from the intraperitoneal space (which is separated from the retroperitoneum by the posterior peritoneal lining). This may delay the development of classic symptoms and signs of perforation (eg, fever, diffuse abdominal pain), . In addition, back or flank pain (eg, right flank pain) may be present due to retropentoneal inflammation.
-Aspects of duodenal anatomy that increase the duodenum's susceptibility to perforation include:
. Its location anterior to the vertebral column: compression against the vertebral column during BAT can rapidly increase intraluminal pressure, causing rupture.
. Its multiple attachments (eg, hepatoduodenal ligament, ligament of Treitz): abrupt force against the duodenum can cause duodenal tearing at fixed points of attachment rather than stretching.
C-The stomach and transverse colon are also susceptible to rupture from rapid change in intraluminal pressure during BAT. However, both are intraperitoneal (vs retroperitoneal) structures. Therefore, intraperitoneal free air (eg, free air under the diaphragm on chest x—ray) would be expected on imaging .
BAT can injure the pancreas or kidney, causing spillage of pancreatic enzymes or urine into the retroperitoneal space. Although both renal pelvis laceration and traumatic pancreatitis could result in a delayed presentation of abdominal and right flank pain, they would typically cause free fluid rather than free air on
Treatment / Management
Treatment of patients with blunt abdominal injury requires the routine ABCs (Airway, Breathing, and Circulation). Once the airway is protected, it is mandatory to protect the cervical spine. After the primary survey is complete, patients who are hypotensive require aggressive fluid resuscitation. If hemodynamic instability persists, blood should be typed and crossed, but in the meantime, immediate transfusion with O negative blood can be done (O+ for males and women past childbearing years). All patients with blunt abdominal trauma who have signs of peritonitis, frank bleeding, or worsening of clinical signs require an immediate laparotomy. Non-surgical treatment in patients with blunt abdominal injury depends on the clinical features, hemodynamic stability and results of the CT scan. Advances in angiography can now help control hemorrhage with the use of embolization therapy, which is more cost effective than laparotomy. In general, the prognosis of patients with blunt abdominal trauma is good
References
Authors
Maria C. O'Rourke1; Ryan Landis2; Bracken Burns3
1.
Garside G, Khan O, Mukhtar Z, Sinha C. Paediatric duodenal injury complicated by common bile duct rupture due to blunt trauma: a multispecialist approach. BMJ Case Rep. 2018 Aug 29;2018 [PMC free article] [PubMed]
2.
Zhou H, Ma X, Sheng M, Lai C, Fu J. Evolution of intramural duodenal hematomas on magnetic resonance imaging. Pediatr Radiol. 2018 Oct;48(11):1593-1599. [PubMed]
3.
Molinelli V, Iosca S, Duka E, De Marchi G, Lucchina N, Bracchi E, Carcano G, Novario R, Fugazzola C. Ability of specific and nonspecific signs of multidetector computed tomography (MDCT) in the diagnosis of blunt surgically important bowel and mesenteric injuries. Radiol Med. 2018 Dec;123(12):891-903. [PubMed]
4.
Taghavi S, Askari R. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 22, 2021. Liver Trauma. [PubMed]
5.
Renson A, Musser B, Schubert FD, Bjurlin MA. Seatbelt use is associated with lower risk of high-grade hepatic injury in motor vehicle crashes in a national sample. J Epidemiol Community Health. 2018 Aug;72(8):746-751. [PubMed]
6.
Pelletti G, Cecchetto G, Viero A, De Matteis M, Viel G, Montisci M. Traumatic fatal aortic rupture in motorcycle drivers. Forensic Sci Int. 2017 Dec;281:121-126. [PubMed]
7.
Tarchouli M, Elabsi M, Njoumi N, Essarghini M, Echarrab M, Chkoff MR. Liver trauma: What current management? Hepatobiliary Pancreat Dis Int. 2018 Feb;17(1):39-44. [PubMed]
8.
So HF, Nabi H. Handlebar hernia - A rare complication from blunt trauma. Int J Surg Case Rep. 2018;49:118-120. [PMC free article] [PubMed]
9.
Wortman JR, Uyeda JW, Fulwadhva UP, Sodickson AD. Dual-Energy CT for Abdominal and Pelvic Trauma. Radiographics. 2018 Mar-Apr;38(2):586-602. [PubMed]
10.
Tsai R, Raptis D, Raptis C, Mellnick VM. Traumatic abdominal aortic injury: clinical considerations for the diagnostic radiologist. Abdom Radiol (NY). 2018 May;43(5):1084-1093. [PubMed]
11.
Tomic I, Dragas M, Vasin D, Loncar Z, Fatic N, Davidovic L. Seat-Belt Abdominal Aortic Injury-Treatment Modalities. Ann Vasc Surg. 2018 Nov;53:270.e13-270.e16. [PubMed]
12.
Inukai K, Uehara S, Furuta Y, Miura M. Nonoperative management of blunt liver injury in hemodynamically stable versus unstable patients: a retrospective study. Emerg Radiol. 2018 Dec;25(6):647-652. [PubMed]
13.
Sarychev LP, Sarychev YV, Pustovoyt HL, Sukhomlin SA, Suprunenko SM. Management of the patients with blunt renal trauma: 20 years of clinical experience. Wiad Lek. 2018;71(3 pt 2):719-722. [PubMed]
14.
Cunningham AJ, Lofberg KM, Krishnaswami S, Butler MW, Azarow KS, Hamilton NA, Fialkowski EA, Bilyeu P, Ohm E, Burns EC, Hendrickson M, Krishnan P, Gingalewski C, Jafri MA. Minimizing variance in Care of Pediatric Blunt Solid Organ Injury through Utilization of a hemodynamic-driven protocol: a multi-institution study. J Pediatr Surg. 2017 Dec;52(12):2026-2030. [PubMed]
15.
Aeberhard P, Weber M. [Sigmoid colon injuries caused by blunt abdominal trauma]. Helv Chir Acta. 1979 Feb;45(6):719-22. [PubMed]
16.
Waheed KB, Baig AA, Raza A, Ul Hassan MZ, Khattab MA, Raza U. Diagnostic accuracy of Focused Assessment with Sonography for Trauma for blunt abdominal trauma in the Eastern Region of Saudi Arabia. Saudi Med J. 2018 Jun;39(6):598-602. [PMC free article] [PubMed]
17.
Margari S, Garozzo Velloni F, Tonolini M, Colombo E, Artioli D, Allievi NE, Sammartano F, Chiara O, Vanzulli A. Emergency CT for assessment and management of blunt traumatic splenic injuries at a Level 1 Trauma Center: 13-year study. Emerg Radiol. 2018 Oct;25(5):489-497. [PubMed]
18.
Guillen B, Cassaro S. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 15, 2021. Traumatic Open Abdomen. [PubMed]



